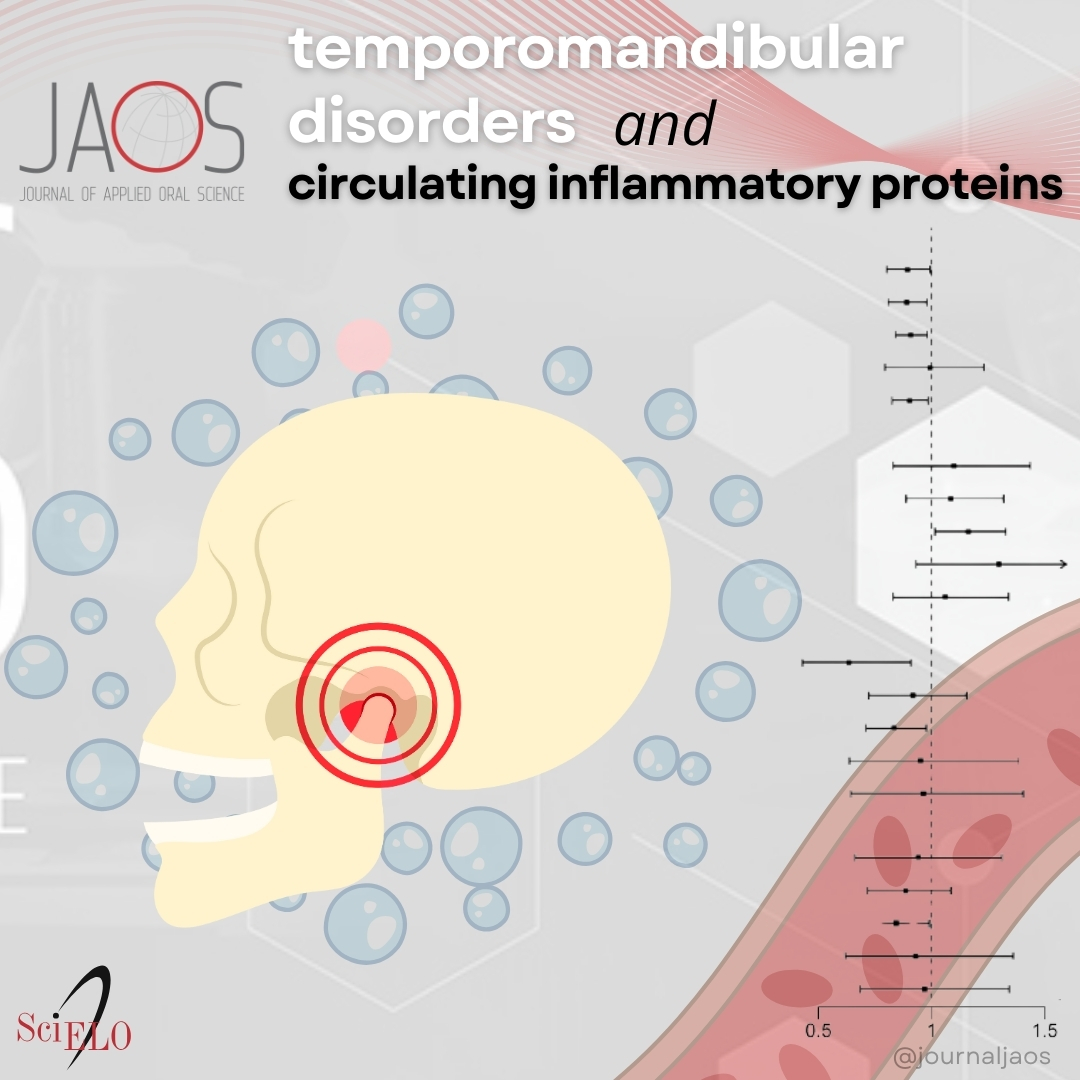
Association between circulating inflammatory proteins and temporomandibular disorders
insight from a two-sample Mendelian randomization analysis
DOI:
https://doi.org/10.1590/1678-7757-2024-0112Keywords:
Mendelian randomization, Circulating inflammatory proteins, Temporomandibular disorders, Genome-wide association studiesAbstract
Background Past studies have indicated links between specific inflammatory proteins in the bloodstream and temporomandibular disorders (TMDs). Nonetheless, there remains the need for further solid research pinpointing the exact causes behind these associations. This Mendelian randomization (MR) study aims to examine the association between 91 circulating inflammatory proteins and TMDs.
Methodology The most comprehensive genome-wide association studies available for circulating inflammatory proteins and TMDs was used in this two-sample MR analysis. The association between genetic predispositions to TMDs and levels of circulating inflammatory proteins was explored by various methods, including inverse variance weighted, MR-Egger, weighted median, simple mode, weighted mode, and MR-PRESSO techniques. To evaluate the reliability of these findings, sensitivity analyses such as Cochran’s Q test, the MR-Egger intercept test, and a leave-one-out approach were conducted.
Results Findings indicated significant links between lower levels of circulating CCL4 (odds ratio, OR: 0.9241, 95% confidence interval, CI: 0.8679-0.984, p=0.0138), IL-20 (OR: 0.8615, 95%CI: 0.7566-0.9808, p=0.0243), and TWEAK (OR: 0.8702, 95%CI: 0.7634-0.992, p=0.0375) and an increased risk of TMDs, according to the inverse variance weighted method. Conversely, a higher level of S100A12 in the blood stream was associated with an increased risk of TMDs (OR: 1.1368, 95%CI: 1.0134-1.2752, p=0.0286). Sensitivity analyses confirmed the stability of these outcomes.
Conclusion This study suggests that reduced levels of CCL4, IL-20, and TWEAK are associated with a higher risk of TMDs, alongside an increased risk of TMDs connected to elevated levels of S100A12.
Downloads
References
- Beaumont S, Garg K, Gokhale A, Heaphy N. Temporomandibular disorder: a practical guide for dental practitioners in diagnosis and management. Aust Dent J. 2020;65(3):172-80. doi: 10.1111/adj.12785
» https://doi.org/10.1111/adj.12785
- Lee E, Crowder HR, Tummala N, Goodman JF, Abbott J, Zapanta PE. Temporomandibular disorder treatment algorithm for otolaryngologists. Am J Otolaryngol. 2021;42(6):103155. doi: 10.1016/j.amjoto.2021.103155
» https://doi.org/10.1016/j.amjoto.2021.103155
- Thomas DC, Eliav E, Garcia AR, Fatahzadeh M. Systemic factors in temporomandibular disorder pain. Dent Clin North Am. 2023;67(2):281-98. doi: 10.1016/j.cden.2022.10.002
» https://doi.org/10.1016/j.cden.2022.10.002
- Schiffman E, Ohrbach R, Truelove E, Look J, Anderson G, Goulet JP, et al. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: recommendations of the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Groupdagger. J Oral Facial Pain Headache. 2014;28(1):6-27. doi: 10.11607/jop.1151
» https://doi.org/10.11607/jop.1151
- Ingawale S, Goswami T. Temporomandibular joint: disorders, treatments, and biomechanics. Ann Biomed Eng. 2009;37(5):976-96. doi: 10.1007/s10439-009-9659-4
» https://doi.org/10.1007/s10439-009-9659-4
- Silva MT, Silva C, Silva J, Costa M, Gadotti I, Ribeiro K. Effectiveness of physical therapy interventions for temporomandibular disorders associated with tinnitus: a systematic review. J Clin Med. 2023;12(13):4329. doi: 10.3390/jcm12134329
» https://doi.org/10.3390/jcm12134329
- Medlicott MS, Harris SR. A systematic review of the effectiveness of exercise, manual therapy, electrotherapy, relaxation training, and biofeedback in the management of temporomandibular disorder. Phys Ther. 2006;86(7):955-73.
- Paço M, Peleteiro B, Duarte J, Pinho T. The Effectiveness of physiotherapy in the management of temporomandibular disorders: a systematic review and meta-analysis. J Oral Facial Pain Headache. 2016;30(3):210-20. doi: 10.11607/ofph.1661
» https://doi.org/10.11607/ofph.1661
- Scrivani SJ, Keith DA, Kaban LB. Temporomandibular disorders. N Engl J Med. 2008;359(25):2693-705. doi: 10.1056/NEJMra0802472
» https://doi.org/10.1056/NEJMra0802472
- List T, Axelsson S. Management of TMD: evidence from systematic reviews and meta-analyses. J Oral Rehabil. 2010;37(6):430-51. doi: 10.1111/j.1365-2842.2010.02089.x
» https://doi.org/10.1111/j.1365-2842.2010.02089.x
- Chisnoiu AM, Picos AM, Popa S, Chisnoiu PD, Lascu L, Picos A, et al. Factors involved in the etiology of temporomandibular disorders: a literature review. Clujul Med. 2015;88(4):473-8. doi: 10.15386/cjmed-485
» https://doi.org/10.15386/cjmed-485
- Svensson P, Kumar A. Assessment of risk factors for oro-facial pain and recent developments in classification: implications for management. J Oral Rehabil. 2016;43(12):977-89. doi: 10.1111/joor.12447
» https://doi.org/10.1111/joor.12447
- Fillingim RB, Slade GD, Greenspan JD, Dubner R, Maixner W, Bair E, et al. Long-term changes in biopsychosocial characteristics related to temporomandibular disorder: findings from the OPPERA study. Pain. 2018;159(11):2403-13. doi: 10.1097/j.pain.0000000000001348
» https://doi.org/10.1097/j.pain.0000000000001348
- Shrivastava M, Battaglino R, Ye L. A comprehensive review on biomarkers associated with painful temporomandibular disorders. Int J Oral Sci. 2021;13(1):23. doi: 10.1038/s41368-021-00129-1
» https://doi.org/10.1038/s41368-021-00129-1
- Jounger SL, Christidis N, Svensson P, List T, Ernberg M. Increased levels of intramuscular cytokines in patients with jaw muscle pain. J Headache Pain. 2017;18(1):30. doi: 10.1186/s10194-017-0737-y
» https://doi.org/10.1186/s10194-017-0737-y
- Nascimento GC, Rizzi E, Gerlach RF, Leite-Panissi CR. Expression of MMP-2 and MMP-9 in the rat trigeminal ganglion during the development of temporomandibular joint inflammation. Braz J Med Biol Res. 2013;46(11):956-67. doi: 10.1590/1414-431X20133138
» https://doi.org/10.1590/1414-431X20133138
- Liao Y, Ren Y, Luo X, Mirando AJ, Long JT, Leinroth A, et al. Interleukin-6 signaling mediates cartilage degradation and pain in posttraumatic osteoarthritis in a sex-specific manner. Sci Signal. 2022;15(744):eabn7082. doi: 10.1126/scisignal.abn7082
» https://doi.org/10.1126/scisignal.abn7082
- Almeida LE, Doetzer A, Beck ML. Immunohistochemical markers of temporomandibular disorders: a review of the literature. J Clin Med. 2023;12(3):789. doi: 10.3390/jcm12030789
» https://doi.org/10.3390/jcm12030789
- Ita ME, Ghimire P, Granquist EJ, Winkelstein BA. MMPs in tissues retrieved during surgery from patients with TMJ disorders relate to pain more than to radiological damage score. J Orthop Res. 2022;40(2):338-47. doi: 10.1002/jor.25048
» https://doi.org/10.1002/jor.25048
- Zhang P, Gan YH. Prostaglandin E(2) upregulated trigeminal ganglionic sodium channel 1.7 involving temporomandibular joint inflammatory pain in rats. Inflammation. 2017;40(3):1102-9. doi: 10.1007/s10753-017-0552-2
» https://doi.org/10.1007/s10753-017-0552-2
- Burgess S, Smith GD, Davies NM, Dudbridge F, Gill D, Glymour MM, et al. Guidelines for performing mendelian randomization investigations: update for summer 2023. Wellcome Open Res. 2023;4:186. doi: 10.12688/wellcomeopenres.15555.3
» https://doi.org/10.12688/wellcomeopenres.15555.3
- Sanderson E, Glymour MM, Holmes MV, Kang H, Morrison J, Munafo MR, et al. Mendelian randomization. Nat Rev Methods Primers. 2022;2:6. doi: 10.1038/s43586-021-00092-5
» https://doi.org/10.1038/s43586-021-00092-5
- Lee CH, Cook S, Lee JS, Han B. Comparison of two meta-analysis methods: inverse-variance-weighted average and weighted sum of Z-scores. Genomics Inform. 2016;14(4):173-80. doi: 10.5808/GI.2016.14.4.173
» https://doi.org/10.5808/GI.2016.14.4.173
- Ibi M. Inflammation and temporomandibular joint derangement. Biol Pharm Bull. 2019;42(4):538-42. doi: 10.1248/bpb.b18-00442
» https://doi.org/10.1248/bpb.b18-00442
- Ulmner M, Sugars R, Naimi-Akbar A, Alstergren P, Lund B. Cytokines in temporomandibular joint synovial fluid and tissue in relation to inflammation. J Oral Rehabil. 2022;49(6):599-607. doi: 10.1111/joor.13321
» https://doi.org/10.1111/joor.13321
- McGeachy MJ, Cua DJ, Gaffen SL. The IL-17 family of cytokines in health and disease. Immunity. 2019;50(4):892-906. doi: 10.1016/j.immuni.2019.03.021
» https://doi.org/10.1016/j.immuni.2019.03.021
- Szewczak L, Donskow-Lysoniewska K. Cytokines and transgenic matrix in autoimmune diseases: similarities and differences. Biomedicines. 2020;8(12):559. doi: 10.3390/biomedicines8120559
» https://doi.org/10.3390/biomedicines8120559
- Mukaida N, Sasaki SI, Baba T. CCL4 Signaling in the Tumor Microenvironment. Adv Exp Med Biol. 2020;1231:23-32. doi: 10.1007/978-3-030-36667-4_3
» https://doi.org/10.1007/978-3-030-36667-4_3
- Sindhu S, Kochumon S, Shenouda S, Wilson A, Al-Mulla F, Ahmad R. The cooperative induction of CCL4 in human monocytic cells by TNF-alpha and palmitate requires MyD88 and involves MAPK/NF-kappaB signaling pathways. Int J Mol Sci. 2019;20(18):4658. doi: 10.3390/ijms20184658
» https://doi.org/10.3390/ijms20184658
- Silva TA, Garlet GP, Fukada SY, Silva JS, Cunha FQ. Chemokines in oral inflammatory diseases: apical periodontitis and periodontal disease. J Dent Res. 2007;86(4):306-19. doi: 10.1177/154405910708600403
» https://doi.org/10.1177/154405910708600403
- Qiao Y, Li J, Yuh C, Ko F, Mercuri LG, Alkhudari J, et al. Chemokine regulation in temporomandibular joint disease: a comprehensive review. Genes (Basel). 2023;14(2):408. doi: 10.3390/genes14020408
» https://doi.org/10.3390/genes14020408
- Watanabe H, Iori T, Lee JW, Kajii TS, Takakura A, Takao-Kawabata R, et al. Association between an increased serum CCL5 level and pathophysiology of degenerative joint disease in the temporomandibular joint in females. Int J Mol Sci. 2023;24(3):2775. doi: 10.3390/ijms24032775
» https://doi.org/10.3390/ijms24032775
- Minervini G, Franco R, Crimi S, Di Blasio M, D'Amico C, Ronsivalle V, et al. Pharmacological therapy in the management of temporomandibular disorders and orofacial pain: a systematic review and meta-analysis. BMC Oral Health. 2024;24(1):78. doi: 10.1186/s12903-023-03524-8
» https://doi.org/10.1186/s12903-023-03524-8
- Zwiri A, Al-Hatamleh MA, Ahmad WM, Asif JA, Khoo SP, Husein A, et al. Biomarkers for temporomandibular disorders: current status and future directions. Diagnostics (Basel). 2020;10(5):303. doi: 10.3390/diagnostics10050303
» https://doi.org/10.3390/diagnostics10050303
- Chiu YS, Hsing CH, Li CF, Lee CY, Hsu YH, Chang MS. Anti-IL-20 monoclonal antibody inhibited tumor growth in hepatocellular carcinoma. Sci Rep. 2017;7(1):17609. doi: 10.1038/s41598-017-17054-1
» https://doi.org/10.1038/s41598-017-17054-1
- Hsu YH, Yang YY, Huwang MH, Weng YH, Jou IM, Wu PT, et al. Anti-IL-20 monoclonal antibody inhibited inflammation and protected against cartilage destruction in murine models of osteoarthritis. PLoS One. 2017;12(4):e0175802. doi: 10.1371/journal.pone.0175802
» https://doi.org/10.1371/journal.pone.0175802
- Lin TY, Hsu YH. IL-20 in acute kidney injury: role in pathogenesis and potential as a therapeutic target. Int J Mol Sci. 2020;21(3):1009. doi: 10.3390/ijms21031009
» https://doi.org/10.3390/ijms21031009
- Abos B, Perez-Fernandez E, Morel E, Perdiguero P, Tafalla C. Pro-inflammatory and B cell regulating capacities of TWEAK in rainbow trout ( Oncorhynchus mykiss ). Front Immunol. 2021;12:748836. doi: 10.3389/fimmu.2021.748836
» https://doi.org/10.3389/fimmu.2021.748836
- Yamana J, Morand EF, Manabu T, Sunahori K, Takasugi K, Makino H, et al. Inhibition of TNF-induced IL-6 by the TWEAK-Fn14 interaction in rheumatoid arthritis fibroblast like synoviocytes. Cell Immunol. 2012;272(2):293-8. doi: 10.1016/j.cellimm.2011.09.004
» https://doi.org/10.1016/j.cellimm.2011.09.004
- Pietzsch J, Hoppmann S. Human S100A12: a novel key player in inflammation? Amino Acids. 2009;36(3):381-9. doi: 10.1007/s00726-008-0097-7
» https://doi.org/10.1007/s00726-008-0097-7
- Witarto BS, Visuddho V, Witarto AP, Sampurna MTA, Irzaldy A. Performance of fecal S100A12 as a novel non-invasive diagnostic biomarker for pediatric inflammatory bowel disease: a systematic review and meta-analysis. J Pediatr (Rio J). 2023;99(5):432-42. doi: 10.1016/j.jped.2023.03.002
» https://doi.org/10.1016/j.jped.2023.03.002
- Chung YM, Goyette J, Tedla N, Hsu K, Geczy CL. S100A12 suppresses pro-inflammatory, but not pro-thrombotic functions of serum amyloid A. PLoS One. 2013;8(4):e62372. doi: 10.1371/journal.pone.0062372
» https://doi.org/10.1371/journal.pone.0062372
- Nishida M, Saegusa J, Tanaka S, Morinobu A. S100A12 facilitates osteoclast differentiation from human monocytes. PLoS One. 2018;13(9):e0204140. doi: 10.1371/journal.pone.0204140
Downloads
Published
Versions
- 2025-01-14 (2)
- 2025-01-10 (1)
Issue
Section
License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Todo o conteúdo do periódico, exceto onde está identificado, está licenciado sob uma Licença Creative Commons do tipo atribuição CC-BY.

