The action of microbial collagenases in dentinal matrix degradation in root caries and potential strategies for its management: a comprehensive state-of-the-art review
DOI:
https://doi.org/10.1590/1678-7757-2024-0013Keywords:
Dental caries, Root caries, Collagenases, Microbial collagenase, Matrix metalloproteinasesAbstract
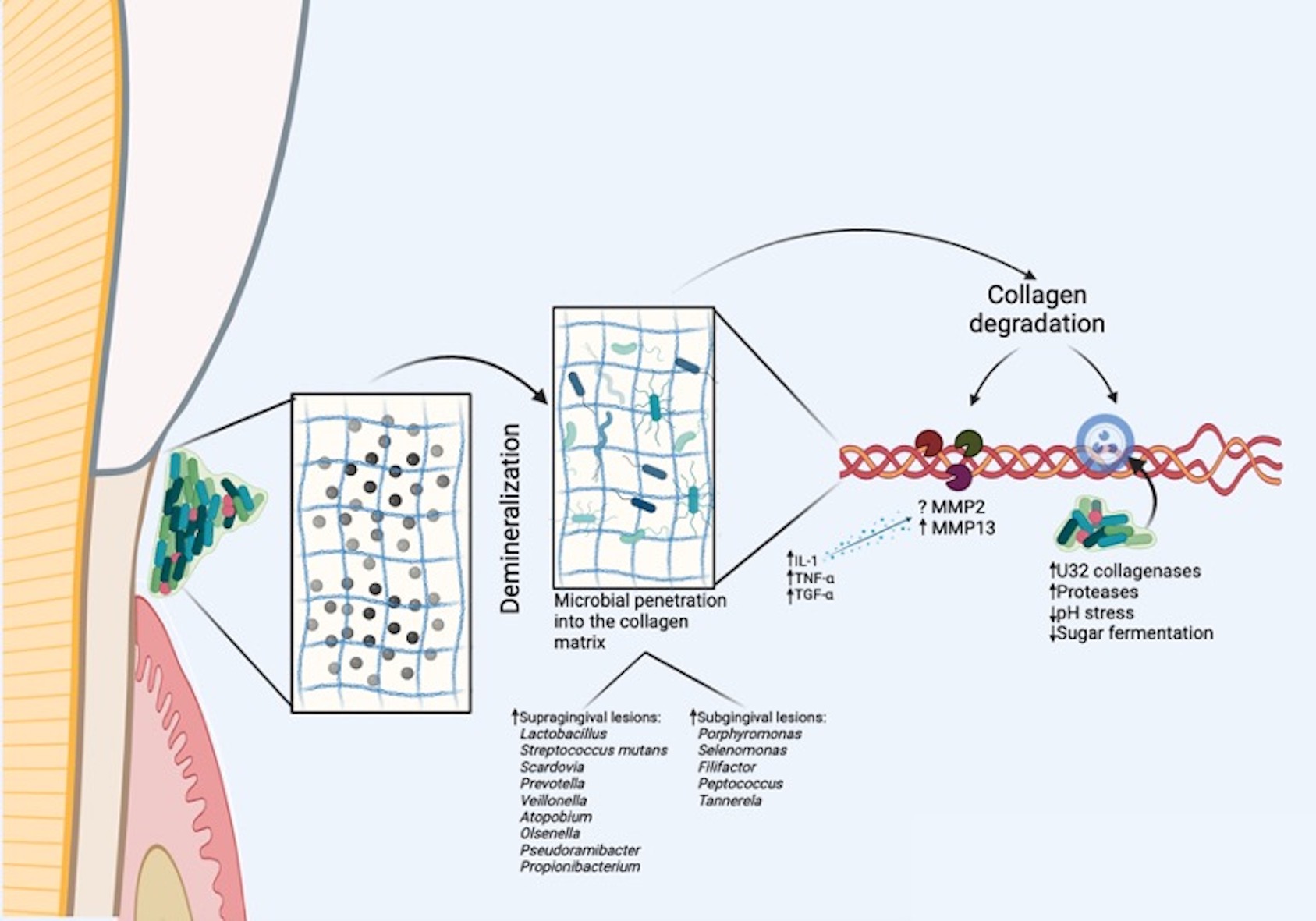
Conventional views associate microbial biofilm with demineralization in root caries (RC) onset, while research on their collagenases role in the breakdown of collagen matrix has been sporadically developed, primarily in vitro. Recent discoveries, however, reveal proteolytic bacteria enrichment, specially Porphyromonas and other periodontitis-associated bacteria in subgingivally extended lesions, suggesting a potential role in RC by the catabolism of dentin organic matrix. Moreover, genes encoding proteases and bacterial collagenases, including the U32 family collagenases, were found to be overexpressed in both coronal and root dentinal caries. Despite these advancements, to prove microbial collagenolytic proteases’ definitive role in RC remains a significant challenge. A more thorough investigation is warranted to explore the potential of anti-collagenolytic agents in modulating biofilm metabolic processes or inhibiting/reducing the size of RC lesions. Prospective treatments targeting collagenases and promoting biomodification through collagen fibril cross-linking show promise for RC prevention and management. However, these studies are currently in the in vitro phase, necessitating additional research to translate findings into clinical applications. This is a comprehensive state-of-the-art review aimed to explore contributing factors to the formation of RC lesions, particularly focusing on collagen degradation in root tissues by microbial collagenases.
Downloads
References
Hayes M, Burke F, Allen PF. Incidence, prevalence and global distribution of root caries. Monogr Oral Sci. 2017;26:1-8. doi: 10.1159/000479301
Hariyani N, Setyowati D, Spencer AJ, Luzzi L, Do LG. Root caries incidence and increment in the population - a systematic review, meta-analysis and meta-regression of longitudinal studies. J Dent. 2018;77:1-7. doi: 10.1016/j.jdent.2018.06.013
Griffin SO, Griffin PM, Swann JL, Zlobin N. Estimating rates of new root caries in older adults. J Dent Res. 2004;83(8):634-8. doi: 10.1177/154405910408300810
Damé-Teixeira N, Parolo CC, Maltz M. Specificities of caries on root surface. Monogr Oral Sci. 2017;26:15-25. doi: 10.1159/000479303
Reis A, Soares PV, de Geus J, Loguercio AD. Clinical performance of root surface restorations. Monogr Oral Sci. 2017;26:115-24. doi: 10.1159/000479353
Gostemeyer G, Mata C, McKenna G, Schwendicke F. Atraumatic vs conventional restorative treatment for root caries lesions in older patients: meta- and trial sequential analysis. Gerodontology. 2019;36(3):285-93. doi: 10.1111/ger.12409
Burrow MF, Stacey MA. Management of cavitated root caries lesions: minimum intervention and alternatives. Monogr Oral Sci. 2017;26:106-14. doi: 10.1159/000479352
Wierichs RJ, Meyer-Lueckel H. Response to letter to the editor, “Systematic review on noninvasive treatment of root caries lesions”. J Dent Res. 94. 2015. doi: 10.1177/0022034515591480
Meyer-Lueckel H, Machiulskiene V, Giacaman RA. How to intervene in the root caries process? Systematic review and meta-analyses. Caries Res;2019. p. 1-10. doi: 10.1159/000501588
Paris S, Banerjee A, Bottenberg P, Breschi L, Campus G, Doméjean S, et al. How to intervene in the caries process in older adults: a joint ORCA and EFCD expert Delphi Consensus Statement. Caries Res. 2020;54(5-6):1-7. doi: 10.1159/000510
Dame-Teixeira N, Parolo CC, Maltz M, Tugnait A, Devine D, Do T. Actinomyces spp. gene expression in root caries lesions. J Oral Microbiol. 2016;8:32383. doi: 10.3402/jom.v8.32383
Damé-Teixeira N, Parolo C, Maltz M, Rup A, Devine D, Do T. Gene expression of bacterial collagenolytic proteases in root caries. J Oral 10-Microb. 2018;10:1424475. doi: 10.1080/20002297.2018.1424475
Santos HS, Do T, Parolo CC, Poloni JF, Maltz M, Arthur RA, et al. Streptococcus mutans gene expression and functional profile in root caries: an RNA-Seq study. Caries Res. 2022;56(2):116-28. doi: 10.1159/000524196
Santos HS, Damé-Teixeira N, Nagano MH, Do T, Parolo CC, Maltz M, et al. Acid tolerance of Lactobacillus spp. on root carious lesions: a complex and multifaceted response. Arch Oral Biol. 2023;156:105820. doi: 10.1016/j.archoralbio.2023.105820
Barbosa CB, Monici Silva I, Cena JA, Stefani CM, Dame-Teixeira N. Presence of host and bacterial-derived collagenolytic proteases in carious dentin: a systematic review of ex vivo studies. Front Cell Infect Microbiol. 2023;13:1278754. doi: 10.3389/fcimb.2023.1278754
Goldberg M, Kulkarni AB, Young M, Boskey A. Dentin: structure, composition and mineralization. Front Biosci (Elite Ed). 2011 Jan 1;3:711-35. doi: 10.2741/e281
Bosshardt DD, Selvig KA. Dental cementum: the dynamic tissue covering of the root. Periodontol 2000. 1997;13:41-75. doi: 10.1111/j.1600-0757.1997.tb00095.x
Hoppenbrouwers PM, Driessens FC, Borggreven JM. The vulnerability of unexposed human dental roots to demineralization. J Dent Res. 1986;65(7):955-8. doi: 10.1177/00220345860650071101
Klimuszko E, Orywal K, Sierpinska T, Sidun J, Golebiewska M. Evaluation of calcium and magnesium contents in tooth enamel without any pathological changes: in vitro preliminary study. Odontology. 2018;106(4):369-76. doi: 10.1007/s10266-018-0353-6
Teruel JD, Alcolea A, Hernández A, Ruiz AJ. Comparison of chemical composition of enamel and dentine in human, bovine, porcine and ovine teeth. Arch Oral Biol. 2015;60(5):768-75. doi: 10.1016/j.archoralbio.2015.01.014
Christner P, Robinson P, Clark CC. A preliminary characterization of human cementum collagen. Calcif Tissue Res. 1977;23(2):147-50. doi: 10.1007/BF02012780
Breschi L, Maravic T, Cunha SR, Comba A, Cadenaro M, Tjäderhane L, et al. Dentin bonding systems: from dentin collagen structure to bond preservation and clinical applications. Dent Mater. 2018;34(1):78-96.
Shoulders MD, Raines RT. Collagen structure and stability. Annu Rev Biochem. 2009;78:929-58. doi: 10.1016/j.dental.2017.11.005
Ricard-Blum S, Ruggiero F. The collagen superfamily: from the extracellular matrix to the cell membrane. Pathol Biol (Paris). 2005;53(7):430-42. doi: 10.1016/j.patbio.2004.12.024
Ricard-Blum S. The collagen family. Cold Spring Harb Perspect Biol. 2011;3(1):a004978. doi: 10.1101/cshperspect.a004978
Gelse K, Pöschl E, Aigner T. Collagens--structure, function, and biosynthesis. Adv Drug Deliv Rev. 2003;55(12):1531-46. doi: 10.1016/j.addr.2003.08.002
Hulmes DJ, Miller A. Quasi-hexagonal molecular packing in collagen fibrils. Nature. 1979;282(5741):878-80. doi: 10.1038/282878a0
Varma S, Orgel JP, Schieber JD. Nanomechanics of Type I Collagen. Biophys J. 2016;111(1):50-6. doi: 10.1016/j.bpj.2016.05.038
Takahashi N, Nyvad B. Ecological hypothesis of dentin and root caries. Caries Res. 2016;50(4):422-31. doi: 10.1159/000447309
Gross EL, Beall CJ, Kutsch SR, Firestone ND, Leys EJ, Griffen AL. Beyond Streptococcus mutans: dental caries onset linked to multiple species by 16S rRNA community analysis. PLoS One. 2012;7(10). doi: 10.1371/journal.pone.004772231- Do T, Damé-Teixeira N, Naginyte M, Marsh PD. Root surface biofilms and caries. Monogr Oral Sci. 2017;26:26-34. doi: 10.1159/00047
Marsh PD. Microbiology of dental plaque biofilms and their role in oral health and caries. Dent Clin North Am. 2010;54(3):441-54. doi: 10.1016/j.cden.2010.03.002
Takahashi N, Nyvad B. The role of bacteria in the caries process: ecological perspectives. J Dent Res. 2011;90(3):294-303. doi: 10.1177/0022034510379602
Nyvad B, Fejerskov O. An ultrastructural study of bacterial invasion and tissue breakdown in human experimental root-surface caries. J Dent Res. 1990;69(5):1118-25. doi: 10.1177/00220345900690050101
Deyhle H, Bunk O, Muller B. Nanostructure of healthy and caries-affected human teeth. Nanomedicine. 2011;7(6):694-701. doi: 10.1016/j.nano.2011.09.005
Tjaderhane L, Buzalaf MA, Carrilho M, Chaussain C. Matrix metalloproteinases and other matrix proteinases in relation to cariology: the era of ‘dentin degradomics’. Caries Res. 2015;49(3):193-208. doi: 10.1159/000363582
Birkedal-Hansen H. Role of matrix metalloproteinases in human periodontal diseases. J Periodontol. 1993;64(5 Suppl):474-84. doi: 10.1902/jop.1993.64.5s.474
Simon-Soro A, Belda-Ferre P, Cabrera-Rubio R, Alcaraz LD, Mira A. A tissue-dependent hypothesis of dental caries. Caries Res. 2013;47(6):591-600. doi: 10.1159/000351663
Watanabe-Nakayama T, Itami M, Kodera N, Ando T, Konno H. High-speed atomic force microscopy reveals strongly polarized movement of clostridial collagenase along collagen fibrils. Sci Rep. 2016;6:28975. doi: 10.1038/srep28975
Harrington DJ. Bacterial collagenases and collagen-degrading enzymes and their potential role in human disease. Infect Immun. 1996;64(6):1885-91. doi: 10.1128/iai.64.6.1885-1891.1996
Zhang YZ, Ran LY, Li CY, Chen XL. Diversity, structures, and collagen-degrading mechanisms of bacterial collagenolytic proteases. Appl Environ Microbiol. 2015;81(18):6098-107. doi: 10.1128/AEM.00883-15
Kato MT, Leite AL, Hannas AR, Calabria MP, Magalhães AC, Pereira JC, et al. Impact of protease inhibitors on dentin matrix degradation by collagenase. J Dent Res. 2012;91(12):1119-23. doi: 10.1177/0022034512455801
Philominathan ST, Koide T, Matsushita O, Sakon J. Bacterial collagen-binding domain targets undertwisted regions of collagen. Protein Sci. 2012;21(10):1554-65. doi: 10.1002/pro.2145
Vidal CM, Tjäderhane L, Scaffa PM, Tersariol IL, Pashley D, Nader HB, et al. Abundance of MMPs and cysteine cathepsins in caries-affected dentin. J Dent Res. 2014;93(3):269-74. doi: 10.1177/0022034513516979
Welgus HG, Jeffrey JJ, Eisen AZ. Human skin fibroblast collagenase. Assessment of activation energy and deuterium isotope effect with collagenous substrates. J Biol Chem. 1981;256(18):9516-21.
Aas JA, Griffen AL, Dardis SR, Lee AM, Olsen I, Dewhirst FE, et al. Bacteria of dental caries in primary and permanent teeth in children and young adults. J Clin Microbiol. 2008;46(4):1407-17. doi: 10.1128/JCM.01410-07
Preza D, Olsen I, Aas JA, Willumsen T, Grinde B, Paster BJ. Bacterial profiles of root caries in elderly patients. J Clin Microbiol. 2008;46(6):2015-21. doi: 10.1128/JCM.02411-07
Hashimoto K, Sato T, Shimauchi H, Takahashi N. Profiling of dental plaque microflora on root caries lesions and the protein-denaturing activity of these bacteria. Am J Dent. 2011;24(5):295-9.
Takenaka S, Edanami N, Komatsu Y, Nagata R, Naksagoon T, Sotozono M, et al. Periodontal pathogens inhabit root caries lesions extending beyond the gingival margin: a next-generation sequencing analysis. Microorganisms. 2021;9(11). doi: 10.3390/microorganisms9112349
Nyvad B, Takahashi N. Integrated hypothesis of dental caries and periodontal diseases. J Oral Microbiol. 2020;12(1):1710953. doi: 10.1080/20002297.2019.171095
Syed SA, Loesche WJ, Pape HL Jr, Grenier E. Predominant cultivable flora isolated from human root surface caries plaque. Infect Immun. 1975;11(4):727-31. doi: 10.1128/iai.11.4.727-731.1975
Van Strijp AJ, Klont B, Ten Cate JM. Solubilization of dentin matrix collagen in situ. J Dent Res. 1992;71(8):1498-502. doi: 10.1177/00220345920710080701
van Strijp AJ, Jansen DC, DeGroot J, ten Cate JM, Everts V. Host-derived proteinases and degradation of dentine collagen in situ. Caries Res. 2003;37(1):58-65. doi: 10.1159/000068223
van Strijp AJ, Takatsuka T, Sono R, Iijima Y. Inhibition of dentine collagen degradation by hesperidin: an in situ study. Eur J Oral Sci. 2015;123(6):447-52. doi: 10.1111/eos.12225
van Strijp AJ, van Steenbergen TJ, de Graaff J, ten Cate JM. Bacterial colonization and degradation of demineralized dentin matrix in situ. Caries Res. 1994;28(1):21-7. doi: 10.1159/000261615
Ajdic D, McShan WM, McLaughlin RE, Savic G, Chang J, Carson MB, et al. Genome sequence of Streptococcus mutans UA159, a cariogenic dental pathogen. Proc Natl Acad Sci U S A. 2002;99(22):14434-9. doi: 10.1073/pnas.172501299
Navais R, Méndez J, Pérez-Pascual D, Cascales D, Guijarro JA. The yrpAB operon of Yersinia ruckeri encoding two putative U32 peptidases is involved in virulence and induced under microaerobic conditions. Virulence. 2014;5(5):619-24. doi: 10.4161/viru.29363
Kato T, Takahashi N, Kuramitsu HK. Sequence analysis and characterization of the Porphyromonas gingivalis prt C gene, which expresses a novel collagenase activity. J Bacteriol. 1992;174(12):3889-95. doi: 10.1128/jb.174.12.3889-3895.1992
Kawasaki K, Featherstone JD. Effects of collagenase on root demineralization. J Dent Res. 1997;76(1):588-95. doi: 10.1177/00220345970760011001
Tjäderhane L, Larjava H, Sorsa T, Uitto VJ, Larmas M, Salo T. The activation and function of host matrix metalloproteinases in dentin matrix breakdown in caries lesions. J Dent Res. 1998;77(8):1622-9. doi: 10.1177/00220345980770081001
Rosengren L, Winblad B. Proteolytic activity of Streptococcus mutans (GS-5). Oral Surg Oral Med Oral Pathol. 1976;42(6):801-9. doi: 10.1016/0030-4220(76)90103-1
Bowden GH. Microbiology of root surface caries in humans. J Dent Res. 1990;69(5):1205-10. doi: 10.1177/00220345900690051701
Ellen RP, Banting DW, Fillery ED. Streptococcus mutansand Lactobacillus detection in the assessment of dental root surface caries risk. J Dent Res. 1985;64(10):1245-9. doi: 10.1177/00220345850640101301
Nyvad B, Kilian M. Microflora associated with experimental root surface caries in humans. Infect Immun. 1990;58(6):1628-33. doi: 10.1128/iai.58.6.1628-1633
Barbosa CB, Salles LP, Dame-Teixeira N. Isolamento e construção de cassetes de inativação de genes codificadores de colagenases de Streptococcus mutans com possível envolvimento na degradação colagenolítica em Cárie Radicular [Dissertação]: University of Brasilia; 2020.
Schwendicke F, Gostemeyer G. Cost-effectiveness of root caries preventive treatments. J Dent. 2017;56:58-64. doi: 10.1016/j.jdent.2016.10.016
Mellberg JR, Sanchez M. Remineralization by a monofluorophosphate dentifrice in vitro of root dentin softened by artificial caries. J Dent Res. 1986;65(7):959-62. doi: 10.1177/00220345860650071201
Clarkson BH, Rafter ME. Emerging methods used in the prevention and repair of carious tissues. J Dent Educ. 2001;65(10):1114-20.
Baysan A, Lynch E, Ellwood R, Davies R, Petersson L, Borsboom P. Reversal of primary root caries using dentifrices containing 5,000 and 1,100 ppm fluoride. Caries Res. 2001;35(1):41-6. doi: 10.1159/000047429
Wierichs RJ, Meyer-Lueckel H. Systematic review on noninvasive treatment of root caries lesions. J Dent Res. 2015;94(2):261-71. doi: 10.1177/0022034514557330
Araújo MS, Souza LC, Apolonio FM, Barros LO, Reis A, Loguercio AD, et al. Two-year clinical evaluation of chlorhexidine incorporation in two-step self-etch adhesive. J Dent. 2015;43(1):140-8. doi: 10.1016/j.jdent.2014.07.010
Montagner AF, Perroni AP, Corrêa MB, Masotti AS, Pereira-Cenci T, Cenci MS. Effect of pre-treatment with chlorhexidine on the retention of restorations: a randomized controlled trial. Braz Dent J. 2015;26(3):234-41. doi: 10.1590/0103-6440201300009
Cai L, Wu CD. Compounds from Syzygium aromaticum possessing growth inhibitory activity against oral pathogens. J Nat Prod. 1996;59(10):987-90. doi: 10.1021/np960451q
Li XC, Cai L, Wu CD. Antimicrobial compounds from Ceanothus americanus against oral pathogens. Phytochemistry. 1997;46(1):97-102. doi: 10.1016/s0031-9422(97)00222-7.
Chu JP, Li JY, Hao YQ, Zhou XD. Effect of compounds of Galla chinensis on remineralisation of initial enamel carious lesions in vitro. J Dent. 2007;35(5):383-7. doi: 10.1016/j.jdent.2006.11.007
Wang Y, Green A, Yao X, Liu H, Nisar S, Gorski JP, et al. Cranberry juice extract rapidly protects demineralized dentin against digestion and Inhibits Its Gelatinolytic Activity. Materials (Basel). 2021;14(13). doi: 10.3390/ma14133637
Dame-Teixeira N, El-Gendy R, Monici Silva I, Holanda CA, Oliveira AS, Romeiro LAS, et al. Sustainable multifunctional phenolic lipids as potential therapeutics in Dentistry. Sci Rep. 2022;12(1):9299. doi: 10.1038/s41598-022-13292-0
Walter R, Miguez PA, Arnold RR, Pereira PN, Duarte WR, Yamauchi M. Effects of natural cross-linkers on the stability of dentin collagen and the inhibition of root caries in vitro. Caries Res. 2008;42(4):263-8. doi: 10.1159/000135671
Knott L, Bailey AJ. Collagen cross-links in mineralizing tissues: a review of their chemistry, function, and clinical relevance. Bone. 1998;22(3):181-7. doi: 10.1016/s8756-3282(97)00279-2
Bedran-Russo AK, Castellan CS, Shinohara MS, Hassan L, Antunes A. Characterization of biomodified dentin matrices for potential preventive and reparative therapies. Acta Biomater. 2011;7(4):1735-41. doi: 10.1016/j.actbio.2010.12.013
Tezvergil-Mutluay A, Mutluay MM, Agee KA, Seseogullari-Dirihan R, Hoshika T, Cadenaro M, et al. Carbodiimide cross-linking inactivates soluble and matrix-bound MMPs, in vitro. J Dent Res. 2012;91(2):192-6. doi: 10.1177/0022034511427705
Scheffel DL, Hebling J, Scheffel RH, Agee KA, Cadenaro M, Turco G, et al. Stabilization of dentin matrix after cross-linking treatments, in vitro. Dent Mater. 2014;30(2):227-33. doi: 10.1016/j.dental.2013.11.007
Han B, Jaurequi J, Tang BW, Nimni ME. Proanthocyanidin: a natural crosslinking reagent for stabilizing collagen matrices. J Biomed Mater Res A. 2003;65(1):118-24. doi: 10.1002/jbm.a.1046084- Xie Q, Bedran-Russo AK, Wu CD. In vitro remineralization effects of grape seed extract on artificial root caries. J Dent. 2008;36(11):900-6. doi: 10.1016/j.jdent.2008.07.011
Downloads
Published
Issue
Section
License
Copyright (c) 2024 Journal of Applied Oral Science

This work is licensed under a Creative Commons Attribution 4.0 International License.
Todo o conteúdo do periódico, exceto onde está identificado, está licenciado sob uma Licença Creative Commons do tipo atribuição CC-BY.

